Ventricular Septal Defect – Hole between lower chambers of heart

By Justin
A ventricular septal defect (VSD) — sometimes referred to as a hole in the heart — is a type of congenital heart defect in which there is an abnormal opening in the dividing wall between the main pumping chambers of the heart (the ventricles). VSDs are the most common congenital heart defect, and in most cases they’re diagnosed and treated successfully with few or no complications.
What Is a Ventricular Septal Defect?
To understand this defect, it first helps to review some basics about the way a healthy heart typically works.
The heart has four chambers: The two lower pumping chambers of the heart are called the ventricles, and the two upper filling chambers are the atria.
In a typical healthy heart, blood that returns from the body to the right-sided filling chamber (right atrium) is low in oxygen. This blood passes to the right-sided pumping chamber (right ventricle), and then travels to the lungs to receive oxygen. The blood that has been enriched with oxygen returns to the left atrium, and then to the left ventricle. It’s then pumped out to the body through the aorta, a large blood vessel that carries the blood to the smaller blood vessels in the body.
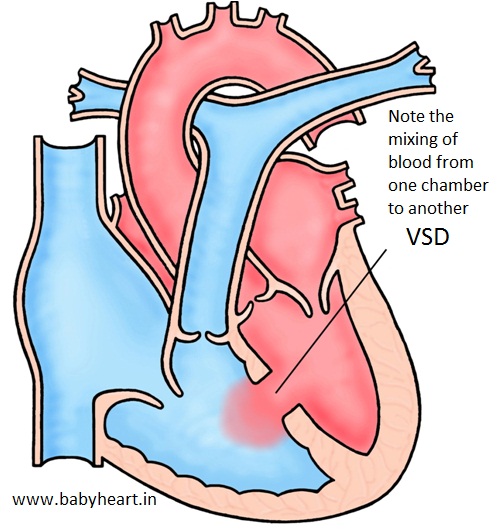
The right and left-sided pumping chambers (ventricles) are separated by shared wall, called the ventricular septum.
Kids with a VSD have an opening in this wall. As a result, when the heart beats, some of the blood in the left ventricle (which has been enriched by oxygen from the lungs) is able to flow through the hole in the septum into the right ventricle. In the right ventricle, this oxygen-rich blood mixes with the oxygen-poor blood and goes back to the lungs. The blood flowing through the hole creates an extra noise, which is known as a heart murmur. The heart murmur, can be heard when a doctor listens to the heart beat with a stethoscope.
VSDs can be located in different places on the ventricular septum, and they can be different sizes. The symptoms and medical treatment of the VSD will depend on those factors. In some rare cases, VSDs are part of more complex types of congenital heart disease.
What Causes a VSD?
Ventricular septal defects occur during fetal heart development and are present at birth. During the first weeks after conception, the heart develops from a large tube, dividing into sections that will eventually become the walls and chambers. If a problem occurs during this process, it can create a hole in the ventricular septum.
In some cases, the tendency to develop a VSD may be genetic. There can be genetic syndromes that cause extra or missing pieces of chromosomes that can be associated with VSD. For the vast majority of children with a defect, however, there’s no clear cause of the VSD.
Signs and Symptoms of a VSD
VSDs are usually found in the first few weeks of life by a doctor during a routine checkup. The doctor will be able to detect a heart murmur, which is due to the sound of blood as it passes between the left and right ventricles. The murmur associated with a VSD has certain features that allow a doctor to distinguish it from heart murmurs due to other causes.
The size of the hole and its location within the heart will determine whether VSD causes any symptoms. Small VSDs will not typically cause any symptoms, and may ultimately close on their own. Older kids or teens who have small VSDs that persist usually don’t experience any symptoms other than the heart murmur that doctors hear. They may need to see a doctor regularly to check on the heart defect and make sure it isn’t causing any problems.
Moderate and large VSDs that haven’t been treated in childhood may cause noticeable symptoms. Babies may have faster breathing and get tired out during attempts to feed. They may start sweating or crying with feeding, and may gain weight at a slower rate.
These signs generally indicate that the VSD will not close by itself, and cardiac surgery may be needed to close the hole. Surgery is typically done within the first 3 months of life to prevent it from causing other complications. A cardiologist can prescribe medication to lessen symptoms before surgery.
People with VSD are at greater risk in their lifetime of developing endocarditis, an infection of the inner surface of the heart. This occurs when bacteria in the bloodstream infect the lining of the heart. Bacteria are always in our mouths, and small amounts are introduced into the bloodstream when we chew and brush our teeth. The best way to protect the heart from endocarditis is to to reduce oral bacteria by brushing and flossing daily, and visiting the dentist regularly. In general, it is not recommended that patients with simple VSDs take antibiotics before dental visits, except for the first 6 months after surgery.
Diagnosing a VSD
If your child is discovered to have a heart murmur that was not noticed earlier, a doctor may refer you to a pediatric cardiologist, a doctor who specializes in diagnosing and treating childhood heart conditions.
In addition to doing a physical exam, the cardiologist take your child’s medical history. If a VSD is suspected, the cardiologist may order one or more of the following tests:
- a chest X-ray, which produces a picture of the heart and surrounding organs
- an electrocardiogram (ECG), which records the electrical activity of the heart
- an echocardiogram (echo), which uses sound waves to produce a picture of the heart and to visualize blood flow through the heart chambers. This is often the primary tool used to diagnose VSD.
- a cardiac catheterization, which provides information about the heart structures as well as blood pressure and blood oxygen levels within the heart chambers. This test is usually performed for VSD only when additional information is needed that other tests cannot provide.
Treating a VSD
Once an VSD is diagnosed, treatment will depend on the child’s age and the size, location, and severity of the defect. A child with a small defect that causes no symptoms may simply need to visit a cardiologist regularly to make sure that there are no other problems. In most children, a small defect will close on its own without surgery. Some may not close, but they do not get any larger. In cases where the VSD is small and has not closed, there are generally no restrictions to activities or to playing sports.
For kids with medium to large VSDs, surgery may be necessary. In most cases, this takes place within the first few weeks to months of life. In this procedure, the surgeon makes an incision in the chest wall, and a heart-lung machine is used to do the work of the circulation while the surgeon closes the hole. The surgeon can stitch the hole closed directly or, more commonly, sew a patch of manmade surgical material over it. Eventually, the tissue of the heart heals over the patch or stitches, and by 6 months after the surgery, the hole will be completely covered with tissue.
Certain types of VSDs may be closed during cardiac catheterization. A thin, flexible tube called a catheter is inserted into a blood vessel in the leg that leads to the heart. A cardiologist guides the tube into the heart to make measurements of blood flow, pressure, and oxygen levels in the heart chambers. A special implant, shaped into two disks formed of flexible wire mesh, can be positioned into the hole in the septum. The device is designed to flatten against the septum on both sides to close and permanently seal the VSD.
After healing from surgery or catheterization, kids with VSDs are considered cured and should have no further symptoms or problems.
Caring for a Child With a VSD
Some kids with VSDs may take heart medication prior to surgery to help lessen the symptoms from the defect. Those who have surgery for larger VSDs usually leave the hospital within 4 to 5 days after surgery if there are no problems.
In most cases, kids who have had VSD surgery recover quickly and without problems. But doctors will closely monitor the child for signs or symptoms of any problems.
Your child may undergo another echocardiogram to make sure that the heart defect has closed completely. If your child is having trouble breathing, call your doctor or take your child to the emergency department immediately. Other symptoms that may indicate a problem include:
- a bluish tinge or color (cyanosis) to the skin around the mouth or on the lips and tongue
- poor appetite or difficulty feeding
- failure to gain weight or weight loss
- listlessness or decreased activity level
- prolonged or unexplained fever
- increasing pain, tenderness, or pus oozing from your child’s incision
Call your doctor if you notice any of these signs in your child after closure of the VSD.
Any time a child is diagnosed with a heart condition, it can be scary. But the good news is that your pediatric cardiologist will be very familiar with this condition and how to best manage it. Most kids who’ve had a VSD corrected have a normal life expectancy and go on to live healthy, active lives.